Glaucoma
Glaucoma is one of the leading causes of blindness. While glaucoma can develop in anyone, people over age 50. Certain types of medical conditions, such as diabetes or extreme near-sightedness, can also increase the risk for glaucoma.
Glaucoma is a term used to describe several types of eye conditions that affect the optic nerve. In many cases, damage to the optic nerve is caused by increased pressure in the eye, also known as intraocular pressure (IOP). Previously it was believed that glaucoma was almost always due to increased intraocular pressure. However, glaucoma can occur in patients with normal and even low eye pressure, so damage to the optic nerve is now key for diagnosis.
Types of Glaucoma
- Primary Open-Angle Glaucoma
- Primary Closed-Angle Glaucoma
- Normal Tension Glaucoma
- Congenital Glaucoma
Recommendations for Glaucoma Screening
- Tonometry and Aplanation Tonometer
- Measurement of Cornea Thickness
- Test for Optic Nerve Damage
- Visual Field(Perimetry) Test
Premier Eye Care was one of the first sites in India to evaluate and implement the progression software called EyeSuite from HAAG-STREIT of Switzerland. Premier Eye Care has patient Visual Field Data spanning 11 years and this gives the patient the benefit of good follow up and management of progressive disease like Glaucoma. Our Optometrists are well versed in making the Patient comfortable and take them through the perimetry step by step.
Visual Fields is an important test conducted for patients on follow up with glaucoma. Glaucoma is a disease which progresses despite medical and surgical intervention. Trials have proved that either may be effective depending on the history, type and stage of glaucoma. The main aim of treatment modality is to retard the progression of glaucoma and make the optic nerve which is the seat of disease (Optic neuropathy) viable for the life of the patient. Visual fields are done once in 4 months when a need to establish the rate of progression of the disease during supervision by the eye surgeon. Computers have helped to evaluate the data generated by the visual field tests and chart the progression and trends for the affected eye. Sensitivity of the eye is measured in decibels and rates of 0.1 decibels per year are unlikely to lead to blindness though this is dependant on when the diagnosis was made.
Decision to Start Treatment
Many people have high IOP but no sign of nerve damage. Over the course of 20 years, only 10 - 30% of these people will actually develop glaucoma. Nevertheless, once glaucoma has destroyed optic nerve fibers, no treatment can reverse the damage.
However, not all individuals with warnings for glaucoma (elevated IOP) develop optic nerve damage and serious vision problems. Nor does treatment prevent progression in some patients. Medications used for glaucoma also can carry side effects and risks.
Medications
Nearly all glaucoma medications are prescribed to reduce eye pressure.
- Beta-blockers (Timolol and Others)
- Prostaglandins
- Carbonic Anhydrase Inhibitors
- Adrenergic Agonists
Managing Drug Regimens
Many patients skip doses of their glaucoma medications, sometimes because of side effects and sometimes because of confusing or time-consuming regimens. Skipping even a few doses can greatly increase the risk of visual loss.
Yag Laser Peripheral Iridotomy
Patients with narrow, occludable angles or who have an attack of acute angle closure glaucoma are treated with Yag laser peripheral iridotomy. Yag PI is done to create a bypass channel for aqueous to flow from behind the iris to the front of the iris, and subsequently into the drainage angle. The procedure typically lasts 10-15 minutes. Prior to the procedure a glaucoma medication is given to prevent any post-laser IOP elevation. In addition, pilocarpine 2% eye drops is given to make the pupil smaller so that the hole can be placed peripherally and make the iris taught. Once the iridotomy is made, it remains open and the risk of acute angle closure glaucoma is eliminated. Even with patent iridotomy hole, patients may still develop increased eye pressure from other mechanisms. These patients are sometimes referred to have mixed mechanism glaucoma. The mechanism is mixed because there is a component of both closed and open angle contributing to the development of glaucoma. Hence a continued follow-up care is required at intervals advised by the eye surgeon.
Filtration Surgery (Trabeculectomy)
The surgeon creates a sclerostomy, a passage in the sclera (the white part of the eye) for draining excess eye fluid. A flap is created that allows fluid to escape without deflating the eyeball. The surgeon may also remove a tiny piece of the iris (called an iridectomy) so that fluid can flow backward into the eye. This surgical procedure is done as a daycare surgery. Trabaculectomy is always combined with wound modulation drug called MMC (Mitomycin C). In the present day Ologen implant is used to modify the scar tissue and create a filtering bed for the new channel of flow for the aqueous (Fluid in the eye) and control the eye pressure safely without having a very soft eyeball after surgery.

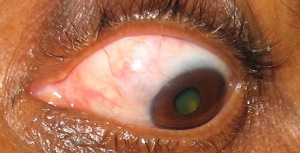
Picture of Trabeculectomy surgery with Ologen Implant Partially absorbed in the eye providing a god scaffold of scar tissue.
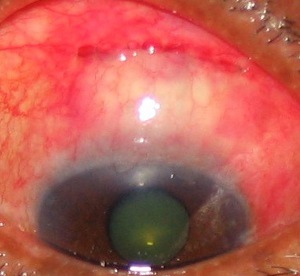
Trabeculectomy+ Mitomycin+ Releasable Suture First Day Postoperative. Note the Bleb Filtering Well
